 Just when you think you’ve got a handle on recent changes to F-tags and survey guidance, a new state issue has people scrambling for information and answers. The Patient Driven Payment Model (PDPM) is coming to state Medicaid programs, and states that used to employ the Resource Utilization Group (RUG) III or IV models are transitioning to this reimbursement model.
Just when you think you’ve got a handle on recent changes to F-tags and survey guidance, a new state issue has people scrambling for information and answers. The Patient Driven Payment Model (PDPM) is coming to state Medicaid programs, and states that used to employ the Resource Utilization Group (RUG) III or IV models are transitioning to this reimbursement model.
One by one, more states are embracing the use of the Medicaid PDPM. If it is not happening in your state, the PDPM is likely on its way like a train coming down the track. The good news is that you can get on board with a ticket for the future and not the baggage of the past.
“People need to pay attention to this because it’s not going away,” said Grant Beebe, DrPH, MBA, NHA, director of Medicaid policy at the American Health Care Association and National Center for Assisted Living (AHCA/NCAL). “The move away from RUGs-III/IV for establishing Medicaid case mix values and the elimination of Section G of the MDS [Minimum Data Set] present an opportunity for greater alignment between reimbursement methodologies and primary cost drivers in long term care.”
Steven Buslovich, MD, CMD, MSHCPM, a practicing medical director and vice president, value-based care, for PointClickCare, observed, “Medicaid programs are undergoing significant changes in the way they're reimbursing nursing homes, particularly with the shift to PDPM, which is being adopted by the states for Medicare reimbursement for the long-stay population. By 2025, all states are expected to transition to this model for Medicaid.”
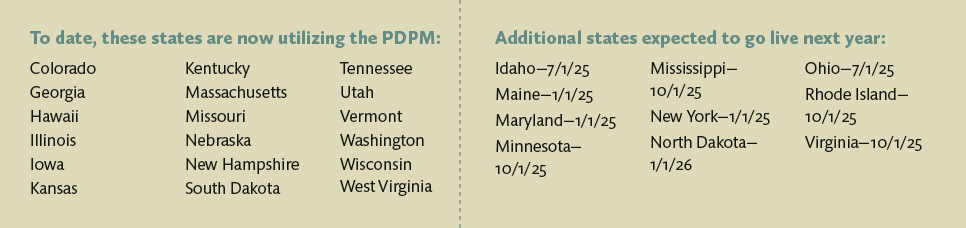
Currently, about 35 states have a case mix system in place, and this is how they’re getting reimbursed for their long term care population. Now that is being replaced with the PDPM, although some states are adopting a hybrid model that includes multiple components, such as nontherapy ancillary services. Several states have already transitioned to the PDPM, and more are expected to follow in the coming months.
 “The impetus behind this move is an attempt at standardization across Medicaid using the same construct so the states are more aligned and we don’t have 15 different models,” said Buslovich.
“The impetus behind this move is an attempt at standardization across Medicaid using the same construct so the states are more aligned and we don’t have 15 different models,” said Buslovich.
Generally, he said, it won’t have an impact on patients/residents or practitioners; it is more about how facilities are getting reimbursed. This will require a greater emphasis on MDS documentation and accuracy. While the MDS coordinator is essential in this effort, the attention of everyone involved in providing documentation that goes into the MDS is also required.
Beebe noted, “We need to make sure that our teams are completing every assessment accurately and that everyone is practicing at the top of their game.” Additionally, data collection and electronic process tools must all support coding on MDS documents.
What Does This Move Mean?
The move to the PDPM will require ensuring that diagnoses are captured accurately on admission and care plans are created accordingly. Previously, care plans were heavily dependent on therapy services, said Buslovich, and moving to the PDPM is likely to have implications for therapy departments. But, he stressed, residents who need therapy services will still be able to get them; they just need to be ordered and documented appropriately. Ultimately, the PDPM is designed to establish a better alignment between the resident’s acuity and the nursing services’ complexity.
This change to state Medicaid programs, Beebe said, also presents an opportunity for fresh content and shared progress in regular facility meetings. “You can use this as a chance to capitalize on the need for collaboration and keeping your whole interdisciplinary team engaged,” he noted. He stressed the importance of talking about your PDPM experiences with your peers and noted, “It is OK for us to scrape our knees as long as we’re willing to learn from one another. This is about doing things right, not being perfect, as long as we’re willing to learn from each other and from our mistakes.”
If the PDPM is to be effective in state Medicaid programs, it will require data-driven decision-making that aligns with the needs of long term care residents. Ideally, this process will be guided by a systematic assessment of Health Insurance Prospective Payment System (HIPPS) codes generated following revisions made to the MDS last year. HIPPS codes represent “specific sets of patient characteristic (or case mix groups) health insurers use to make payment determinations under several prospective payment systems,” according to the Centers for Medicare & Medicaid Services (CMS). For the purposes of payment, at least one HIPPS code represents each case mix group and is reported on insurance claims.
To assist in developing realistic, sustainable Medicaid reimbursement policies, AHCA/NCAL has requested that the Medicaid and CHIP Payment and Access Commission (MACPAC), a federal agency that provides policy and data analysis, encourage state Medicaid agencies to share Medicaid HIPPS codes from October 2023 to the present with the association’s state affiliates.
“This collaboration will enable the partnership to align state priorities and provider needs,” said Beebe. “As we have begun to recognize the value of a data-driven decision-making process, we also see the importance of identifying opportunities that are state-specific and responsive to the resources that they have available to them. Our state affiliates are focused on keeping lines of communication with their state Medicaid agencies open and ensure that we are all on the same page.”
Medicaid agencies also need to share the information so state affiliates can determine whether or not reimbursement reflects clinical acuity in a specific and representative way.
As the PDPM was designed to accommodate the clinical complexity of Medicare short-stay residents and move away from a dependency on therapy services, implementing it for Medicaid long-stay residents, who commonly have ongoing chronic conditions, requires some adjustments, such as the use of blended case mix indices or supplemental payments.
Managing the Models
Beebe noted that, moving forward, “we need to try to figure out what the long term care world can do to be more responsive to shared savings initiatives.”
And they need to do it fairly quickly, however, as after October 1, 2025, there will no longer be federal support for states that choose alternative pathways. Beebe noted, “Once we have a solid foundation with Medicaid PDPM, we will have an opportunity to refine it.”
AHCA/NCAL is looking at ways to help states as they move into using this new model. In a recent white paper, A Case for Iterative Policymaking: Assessing Medicaid PDPM Implementation & Operationalization Strategy, AHCA/NCAL experts wrote, “As states either begin their journey toward implementing the Patient Driven Payment Model (PDPM) or consider opportunities to refine their operationalization of the model, it has become increasingly clear that the economic viability of the long term care sector requires intermediate policy measures capable of responsively evolving in tandem with emerging challenges and insights.”
 Blended case mix indices and add-on payments may help address the limitations of the PDPM for the Medicaid long-stay population, Beebe noted. “State Medicaid agencies can develop a more comprehensive reimbursement approach that encompasses the full spectrum of these residents’ care needs by integrating additional case mix indices that involve nontherapy ancillaries, speech and language pathology, and physical/occupational therapy.”
Blended case mix indices and add-on payments may help address the limitations of the PDPM for the Medicaid long-stay population, Beebe noted. “State Medicaid agencies can develop a more comprehensive reimbursement approach that encompasses the full spectrum of these residents’ care needs by integrating additional case mix indices that involve nontherapy ancillaries, speech and language pathology, and physical/occupational therapy.”
This approach, Beebe suggested, will address gaps in the current PDPM structure and help ensure greater recognition of the most common and costly chronic conditions seen in this population, including Alzheimer’s disease and dementia, bariatric care, behavioral health conditions, infectious illness requiring isolation, swallowing difficulties/dysphagia, tracheostomy, traumatic brain injury, and ventilator dependency.
AHCA/NCAL suggests an iterative approach to policymaking, which recognizes that “understanding the full implications of each state’s individual PDPM transition involves navigating uncertainties and responding to an evolving reimbursement landscape through several key activities.” These include problem identification, initial policy drafting, evaluation and analysis, policy refinement, iterative review, and finalization and implementation.
The association proposes intermediate policy measures designed to resolve limitations of the nursing-only case mix model. These measures include ensuring the stability of care services provided to residents who require support provided in a long term care setting, identifying intermediate reimbursement public policy alternatives that prevent over- or undercompensation, and transitioning beyond the PDPM to develop sustainable reimbursement methodologies for long term care services paid by state Medicaid programs and to compensate for the complex care provided in facilities.
The State Experience
 In an ideal world, there would be one way to implement the PDPM in Medicaid programs that could be rolled out in every state. However, as Juli Pascoe, CPA, a partner at Forvis Mazars US in Missouri, noted, “Every state Medicaid program is so very different, and they all have very different programs.
In an ideal world, there would be one way to implement the PDPM in Medicaid programs that could be rolled out in every state. However, as Juli Pascoe, CPA, a partner at Forvis Mazars US in Missouri, noted, “Every state Medicaid program is so very different, and they all have very different programs.
“In the states we've worked with,” she shared, “it's taking a lot of meetings between the state and the associations and the providers and stakeholder work groups to understand the impact of this change. It takes a great deal of education on the providers’ part to enable them to understand how they were completing their quarterly MDS assessments under RUGs versus under a PDPM model.”
She added, “We’ve always strived for MDS accuracy. That’s still key, but there are different drivers facilities need to be aware of that impact payment under PDPM.” She stressed that everyone needs to get on the same page, and that requires a lot of education and communication.
 Pete Van Runkle, executive director of the Ohio Health Care Association, offered some observations from his state’s experiences. “Ohio’s proposal to move to the nursing-only component of PDPM started in July of 2023. We bought some time by putting in places stop-gap methodology that didn't use PDPM at all, but this only runs through June of 2025.”
Pete Van Runkle, executive director of the Ohio Health Care Association, offered some observations from his state’s experiences. “Ohio’s proposal to move to the nursing-only component of PDPM started in July of 2023. We bought some time by putting in places stop-gap methodology that didn't use PDPM at all, but this only runs through June of 2025.”
In the meantime, he said, “we've been attempting to prepare for what the next step is going to look like, and that's involved working with AHCA and hearing what other states are doing.”
Ohio had to get data from the state, said Van Runkle, and that was a bit of an ordeal. “We eventually got the data, and we’ve been able to conduct an analysis to determine what the impact would be on providers and what could be done to mitigate that,” he said.
“It's all about accuracy,” Van Runkle said, “but we also know the people who are doing this work are human, and you only have so much time in the day for these tasks.” It is key, he suggested, to home in on the relevant details and required data and do your best in those areas where you know the greatest impact will be.
Pascoe said it’s too early to tell what impact the PDPM will have on state Medicaid programs. “We don’t have an answer yet because it hasn’t been fully implemented in many states,” she said.
However, she is confident that providers, working with AHCA/NCAL, their state affiliates, and other stakeholders, will work through the challenges. “They have handled many changes. That's the nature of long term care, and they will handle this one. They just have to stay in tune with what's going on in their state and understand how their program is going to be written and developed,” she suggested.
Van Runkle observed that some providers may think the PDPM is better than a case mix methodology, while others will say it’s not. At any rate, he said, “it’s a big change, and that’s what makes it challenging.”
History of PDPM Suggests Future Challenges
The PDPM for Medicaid isn’t a new concept. CMS has discussed its intention to retire the RUG systems since at least 2018, and in 2022, the agency formally kicked off a nationwide effort to integrate the PDPM into RUGs-III and -IV long term care reimbursement methodologies. Then in 2023, Section G of the MDS was replaced with Section GG and other changes. As a result, states that wished to continue using RUG-based case mix systems were required to use an Optional State Assessment through October 1, 2025.
The AHCA/NCAL white paper noted that the PDPM may still have some kinks to work out. It quoted a report commissioned by MACPAC, which read, “The finding that the current PDPM system is not a good measure of predicting care needs for Medicaid patients suggests that it cannot easily be applied to Medicaid-covered nursing facility stays. In order for states to develop new methods of adjusting for patient acuity when it is no longer possible to use a RUG-based system, further analysis will be required to assess whether some of the components of the PDPM system (such as the nursing-related component, which is more similar to RUG-IV than other PDPM components) can be used for Medicaid payment, to develop payment case mix weights that are appropriate for state Medicaid programs, and to examine how particular types of nursing facilities may be affected by changes to acuity adjustment methods.”
One Step Forward
The next 18 months will be critical as state Medicaid agencies, long term care providers, residents, and industry partners work to operationalize the PDPM within case mix states. An optimal Medicaid reimbursement system that aligns quality care and robust reimbursement may not exist yet, so there will be a need for cross-sector collaboration and innovation to develop a reimbursement model capable of accurately capturing the wide array of services provided to the elderly, frail, and disabled Medicaid beneficiaries in long term care communities from state to state.
No one expects facilities to celebrate these changes and jump in with joy. However, determination and ability to take a fresh look at how they do things will help.
“Those facilities that have prioritized collaborations, teamwork, and the coordination of documentation in recent years likely will have an easier time implementing Medicaid PDPM,” Beebe said. “Stay true to your values and take a deep breath. Don’t panic.”
Ultimately, he said, their commitment to quality care and collaboration, as well as their growing acumen at collecting, analyzing, and using data, will serve them well as they adapt to these changes moving forward.